Clinical Guidelines
Healthcare Professionals Guidelines
These indications are for the use of the Abi ProApp for contributing healthcare professionals. They provide guidelines to answer all kinds of questions from Abi’s customers.
To create these guidelines, we have used information from scientific articles, as well as our experience from hundreds of thousands of cases handled by Abi’s healthcare Professionals and monitored by Abi’s medical team.
What is Abi?
Abi Global Health is a company registered in Ireland that provides health services available to users all over the world. Our objective is to be their first source of health services, using mobile technology in the most convenient way.
Abi is the name of the chat interface that receives questions from patients, sends them to the Healthcare Professionals (HCPs) and then sends the healthcare professionals’ answers back to the patients. Technically, Abi is an artificially intelligent agent, or Chatbot, that uses natural language processing technology to turn normal human language into computer commands to operate the service and provide the answer from the physician to the user.
Healthcare Professionals (HCPs) in Abi can be physicians, nurses, physiotherapists or psychologists. When the healthcare professionals receive a question, the patients can see the name of the healthcare professional answering their question. Patients can also see a profile of every healthcare professional with some essential information. This helps us build trust in that the healthcare professional will answer their questions.
From the patient’s viewpoint, they can ask questions either via a chat app (Whatsapp, Telegram, Viber, etc.) or from a website. There are 5 different types of services provided by Abi: micro-consultations, video-consultations, voice-consultations, mental health and prescriptions. First, the patient must choose the type of consultation they want, and after that they are able to send the inquiry.
It is important to keep in mind that not all patients have access to all services provided by Abi (e.g. not all patients can receive prescriptions or can do video-consultations). Therefore, you must be careful, and not refer patients to other services inside Abi.
General rules for all kinds of consultations
Professionalism
- Make the care of the patient your first concern: keep your knowledge and skills up to date, be honest and act with integrity.
- Work within the limits of your competence.
- Treat each patient as an individual: take into account their history and cultural values.
- Refer a patient to another practitioner/ face-to-face consultation when necessary.
Safety
- If the patient presents a serious condition that must be evaluated in a face-to-face consultation, refer them to seek medical attention.
- Respect the patient’s confidentiality at all times.
- You must pay attention to all the information given by the patient and respond honestly to all of their questions and concerns.
- You must give patients the information they want or need in a way they can understand.
- Your answer must be formal, clear and adapted to the level of knowledge of the patient. Avoid using complex medical terminology and make sure that the patient has understood what you have said.
- Be polite and considerate and respect the dignity and privacy of every patient.
- Be empathetic, so that you can build a trusting relationship with the patient.
- You must support patients in caring for themselves to empower them to improve and maintain their health.
- You must not express your personal beliefs (including political, religious or moral beliefs) to patients.
Text-Consultations
A text consultation consists in a text-based consultation where the patients can ask their questions via a chat app or website. They can add attachments (e.g pictures or test results) to the message and ask follow-up questions.
Patients regularly ask for medical advice (treatments, referrals), guidance and information. It is your job to answer respectfully and give the appropriate information so they are adequately informed by a real healthcare professional.
You have no commitment to answer the questions and you can always decline or exit the case and leave it for another healthcare professional if you see you can’t answer appropriately.
Remember that a text-consultation is not a substitute for a face-to-face consultation, your objective is to guide and inform the patient. Therefore, whenever you think a physical exploration is needed or that there may be an emergency, refer the patient to a hospital or give them the tools to get in touch with an emergency service.
Description of the Process
.jpg?width=483&height=505&name=Micro%20consultations%20(1).jpg)
In case of follow-up questions
The patients have the possibility to ask a new question after the first answer. The first healthcare professional to be notified is the same one who provided the previous answer. If after 2 minutes the follow-up question has not yet been claimed, other healthcare professionals will be notified.
In case of follow up questions, it will always be possible to see the entire case from the first question, including the answers provided by other healthcare professionals.
Keep in mind that the patients can ask a limited number of follow-up questions (3 questions & 3 responses per case) when asking questions to the patients. Try to be specific and ask questions back only if necessary.
General considerations
- Greeting patients: Always greet the patient and warmly express that you are available to answer their questions. A best practice is to begin with sentences like "I'm sorry to hear you're not well" or "Thanks for your question".
- Give informative answers: Your answers are expected to be informative and to help the users with the concerns they have about their health. Please remember that you can’t promise to prescribe medication while conducting a simple text consultation.
- Acknowledge the limitations: Always explain that the opinion is given according to the information available.
- Do not assume the identity of the user: In general, the user will remain anonymous, and their questions can be answered by other healthcare professionals, so whenever facing a consultation do not jump to conclusions about the identity of the user.
- Medical Common Sense: Provide information that is in accordance with the information provided by the user. Abi’s health services are intended to be a useful tool for users who have health concerns and need reliable information to help them make decisions.
- Work within the limits of your competence: If you are not able to provide a pertinent answer, or you just don’t have the time, you can skip the question or cancel at any point during the process.
- Always be respectful: Make sure to be respectful to the inquirer but also to previous caregivers; be supportive of a pre-existing relationship.
- Digital Bedside Manner: Use a sober and gentle style for the answers. After hundreds of thousands of cases, we know our users, like most people, don’t like short and sharp answers, even if the user may sometimes provide information using a truncated ‘SMS-style’ of writing.
- Ending the answer: Finish sentences with comforting phrases such as, “I hope this reassures you” or “I hope you feel better”, which we have found our users greatly appreciate.
Strategies to answer medical text-based consultations
Some basic rules will help you to answer questions in a safe and helpful way:
- Keep close to the facts given in the inquiry.
- Answer in the clearest and simplest way possible. This doesn’t mean a short answer, it is important to clarify the answer with an explanation.
- Always try to give an explanation. Most of the time, even when the patients are looking for guidance or when you think they should go to a face-to-face consultation, the patient needs a little information of what might be happening to them.
- Explain medical terms in plain language. Personalise the answer to match the language used by the inquirer and to the perceived knowledge level of the inquirer.
- Avoid trying to diagnose; instead educate, guide and empower. Often the user only needs to know what the next step they should take is.
- If you need more information or clarify the inquiry, ask short and concrete questions to the inquirer.
Form-Based Prescriptions
Description of the process

General considerations
- Read the patient’s information carefully: Pay attention to their age and weight and always read the key findings and the questionnaire to avoid toxicity/ interactions or other patient harm.
- Take into account the patient’s comment on the request: They may give you useful information about what is happening to them.
- Patient’s safety first: If you think it is not safe to prescribe the patient what they are asking for (because you consider that it can be harmful or because it is not appropriate), decline the request and explain the reasons why.
- Base your prescriptions on medical evidence and try to be up-to-date with the recommendations.
- Work within the limits of your competence: If you are not sure about a prescription, leave the request for another physician.
- If you are unsure about interactions or other aspects of prescribing medicines, seek advice from experienced colleagues or look for the information from appropriate sources.
- Make sure your prescription orders are clear and easy to understand.
- If possible, try to give alternatives to the prescription and guidelines for the patient’s health, such as when to go to the hospital for a face-to-face visit.
Considerations for the issuing of prescriptions via text consultation
- Limited indications:
The prescription service offered by Abi is limited to the list of indications shared to each HCP. The list is limited to what we consider safe to prescribe via a text consultation.
If the user is requesting medication for an indication that is not listed, they must be redirected to an in-person consultation or video consultation.
Do not tell the user they can get medication via the Abi prescription service for an indication that does not exist.
- Multiple prescription requests:
At times, it may be necessary to prescribe more than one medication for an indication. The ability to do so may vary depending on local regulations, and
healthcare professionals will be informed of the applicable process in their country.
Where only one medication can be prescribed at a time, it is acceptable to prescribe the first medication and include a note in the instructions advising the user to submit another request for any additional medications they require.
Do not refuse the initial prescription request solely to prompt users to make multiple additional prescription requests.
- Controlled substances, antibiotics and antivirals:
The prescription of controlled substances; i.e., opioids, benzodiazepines, and antidepressants are prohibited on our platform. If uncertain, decline the prescription request and flag the case.
Prescribing oral antibiotics is restricted to specific indications: Cystitis, bacterial vaginosis, malaria prophylaxis. Please refrain from prescribing oral antibiotics for indications not listed.
Under no circumstances should oral antivirals be prescribed. However, topical antivirals may be prescribed for the indication of cold sores.
- Denial of Medications:
If a medication request is denied, please explain the motives. E.g.: “The same medication was already issued within the past 7 days.” “The medication is not available through form-based service.” “The requested medication is inappropriate for the condition.”
Video Consultations
Description of the process
General considerations
- Introduce yourself: Remember that this is the first time you and the patient are meeting, so always be polite, introduce yourself, and greet the patient so you can build a trusting relationship.
- Patient comfort/ ability: The patient’s comfort level with telemedicine might vary, you need to act accordingly to their limitations and concerns.
- Conversation style and approach for understanding: Keep in mind that you do not have the full range of communication tools that you would have during a face-to-face conversation (body language, etc), so you have to make sure that the patient understands all the information you are trying to communicate. Consider slowing down your pace of speech and ensure that the patient has understood the information.
- Limitations: you might need to ask some extra questions in order to compensate for the loss of face-to-face contact (e.g. physical changes may be less apparent).
- Clear guidelines/ recommendations: be very clear in your communication of recommended care plan/ next steps so there are no misunderstandings.
- Write all take-home messages in the summary: make sure to write all the important information that the patient has to know in the report, such as problem recognition, possible diagnosis and recommendations/next steps (if needed).
- Refer all critical calls to emergency services: examples of critical calls include abdominal or chest pain, fever of unknown origin, high fever lasting more than 48h, convulsions, visual alterations and the onset of labor.
- Issuing prescriptions via video consultation: An initial diagnosis can be made after a medical evaluation during video and/or voice consultations. If you consider it necessary, a prescription can be issued, based on your medical opinion.
- Issuing referrals and sick notes via video consultation: Sick notes and referrals can only be issued after a video consultation with the policyholder, being included in the consultation summary. No back-dating is permitted– sick notes are valid only from the consultation date onward.
Considerations for the issuing of prescriptions via video consultations
- Patient Information: Your should gather basic necessary information from the patient during the video consultation to make an informed prescription. This might include current medications, allergies, medical history, and any other relevant details that could impact the prescription.
- Medical Judgement Priority: Prescriptions must be based on your medical judgement during the video consultation.
- Neutral Stance on Prescribing: The decision to prescribe, or not prescribe, should be grounded in the patient's best medical interest, free from any external influences. There should be no preference between branded and unbranded medications.
- Cost-Effective Choices: In situations where there are different options with similar risk-benefit profiles, you are encouraged to opt for the most cost-effective medication. This ensures that patients receive affordable treatment without compromising quality.
Background and setting
When answering a video consultation, it is important to ensure that the environment is adequate to make the patient feel comfortable talking about their concerns and so you can give the best medical advice. Some things to consider are:
- Privacy: You should be in a quiet, private location for the consultation. If this is not possible, use headphones to ensure others can’t hear the patient’s side of the conversation. Make sure that other people are not walking through the area.
- Background: Clear obstacles and distractions. It is best that the patient can see that you are in a professional setting and are alone for the visit.
- Clothing: Dress conservatively and respectfully, the same way you would for an in-office visit.
- Lighting: Be as well-lit as possible for improved eye contact and trust.
- Camera placement: make sure that the patient can see your face and try to make eye contact with the camera, not the patient’s face. If you need to look away, let the patient know why. If you are answering the video consultation with your phone, try to place the phone on top of a solid and stable surface, so the image is not constantly moving.
- Background noise: Minimize background noise to reduce distractions (no music/ tv/ radio or other controllable noise). Let the patient know if background noise on their end is keeping you from fully focusing on their care and provide suggestions for complete focus.
- Focus: Never multitask while answering a video-consultation. Don’t conduct a visit while driving or otherwise occupied.
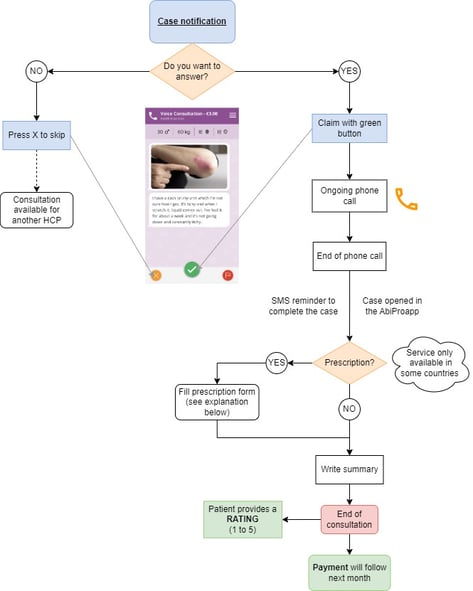
Voice consultations
Description of the process
General considerations
- Greeting patients: Introduce yourself and warmly express to patients that you are happy to speak to them. This interaction will be the first impression that a patient has of you.
- Refer all critical calls to emergency services: Examples of critical calls include abdominal or chest pain, fever of unknown origin, high fever lasting more than 48 hours, convulsions, visual alterations and the onset of labour.
- Clear guidelines/ recommendations: Be very clear in your communication of recommended care plan/ next steps so there are no misunderstandings.
- Write all take-home messages in the summary: Make sure to write all the important information that the patient has to know in the report, such as problem recognition, possible diagnosis and recommendations/next steps, if needed.
- No distractions: Avoid distractions and multi-tasking while answering a telephone consultation.
- Privacy: Maintain the patient’s privacy when communicating over the phone talking from a quiet place that does not allow others to hear any audio.
- Issuing prescriptions via voice consultation: An initial diagnosis can be made after a medical evaluation during video and/or voice consultations. If you consider it necessary, a prescription can be issued at your discretion.
Considerations for the issuing of prescriptions via voice consultations
- Patient Information: Your should gather basic necessary information from the patient during the voice consultation to make an informed prescription. This might include current medications, allergies, medical history, and any other relevant details that could impact the prescription.
- Medical Judgement Priority: Prescriptions must be based on your medical judgement during the voice consultation.
- Neutral Stance on Prescribing: The decision to prescribe, or not prescribe, should be grounded in the patient's best medical interest, free from any external influences. There should be no preference between branded and unbranded medications.
- Cost-Effective Choices: In situations where there are different options with similar risk-benefit profiles, you are encouraged to opt for the most cost-effective medication. This ensures that patients receive affordable treatment without compromising quality.
Strategies to answer medical telephone consultations
- Obtain as much information as possible about the patient’s presenting complaint in a logical sequence as you would do in a face-to-face consultation: never forget to ask about medical history, current medications and allergies to help you arrive at an accurate appraisal of the patient’s condition.
- Ask open-ended questions to elicit sufficient data to assist with decision-making.
- Avoid jumping to conclusions regarding the patient’s situation.
- Listen carefully and allow the caller the time and opportunity to ask questions.
- Speak to patients clearly and slowly, and enunciate carefully.
- Use easy-to-understand language that avoids medical terminology.
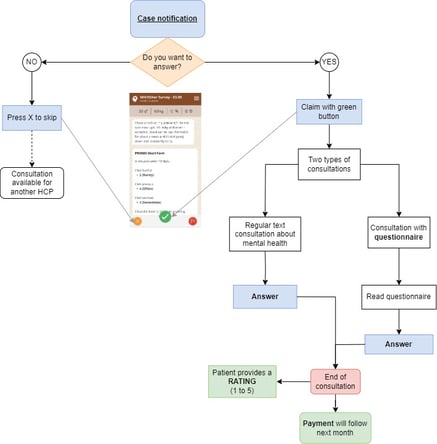
Mental Health consultations
Description of the process
General considerations
- Greeting the patient: Always start the answer by saying hello to the patient to build a relationship in which the patient feels confident and feels that the advice is being given by someone who wants the best for them.
- Explain the findings in the questionnaire to the patient: If the patient has filled a mental health questionnaire, explain to them what the answers might mean.
- Keep close to the facts given in the inquiry.
- Validate the patient’s feelings or symptoms: Express empathy and the understanding of the patient’s feelings and avoid blaming and judging.
- Always be respectful to the inquirer but also to previous caregivers; be supportive of a pre-existing relationship.
- Explain medical terms in plain language: Personalise the answer to match the language used by the inquirer and to the perceived knowledge level of the inquirer.
- Give different solutions or advice to the patient so they know they have options available to cope with their symptoms: Therapies or exercises, medication if needed, referral to a psychologist/ psychiatrist, etc.
- Avoid trying to diagnose and instead, educate, guide and empower. Often the user only needs to know what the next step they should take is.
- If you think the patient’s condition might not be mental health related, but an organic pathology instead, refer the patient to a medical consult.
- Do not give your personal opinion. Always keep the answer professional and based on scientific evidence.
Examples of Frequent Inquiries
|
INQUIRIES |
STRATEGIES |
|
Inquirer worried about a serious condition. |
|
|
You, the healthcare professional, are worried that the inquiry might be related to a serious condition. |
|
|
Inquirer does not fully trust a previous caregiver. |
|
|
Short inquiry with undefined or unclear medical problems. |
|
|
Long and/or confusing inquiries with undefined or unclear medical problems. |
|
|
Answering the “expert inquirer”, who has carried out extensive medical research before submitting the inquiry. |
|
|
Answering inquiries written by someone other than the person the inquiry concerns. |
|
|
Answering inquiries about chronic diseases that have already consulted multiple professionals and have received several lines of treatment, but the symptoms do not improve. |
|
|
The inquirer describes a situation where there is a clear suspicion of harm or abuse being inflicted onto themselves or other persons. |
|
|
The inquirer asks about non-health related matters. |
|
|
Suicidal thoughts / Suicidal ideation (passive): Ideas, or ruminations about the possibility of ending one's life. |
|
|
Active suicidal ideation: The person keeps thinking about dying and even plans how to commit suicide. eg: “I have been thinking about how it would be to jump from a window.“ |
|
|
Suicide threat: Thoughts of killing one’s self that are verbalized to others. eg: “I bought some medication and will take all the pills together tonight” |
|
|
Minors and Dependents |
|
About Our Users
How Do They Find Out About Abi?
Some patients personally buy the service through our website (https://www.abiglobalhealth.com/ ) or through the website of an authorised distributor or partner.
Some patients are offered Abi for free by their health insurance provider, employer, public service or other payer. You will be notified in the question of the origin of the patient (private, insurance, etc).
How Do Users Access Abi?
Abi is not an App that patients download. Rather, Abi is a Chatbot that exists on a patient’s mobile phone as a local telephone number or social media contact. Therefore, patients can access the service through the messaging functionality of apps like Whatsapp, Telegram, Facebook Messenger, Skype, Line, Kik, iPhone & Android Messages or SMS. Some patients also access Abi from within third party health apps which have embedded the Abi Widget into their apps or websites.
Before using the service, the patient accepts our Terms and Conditions which clearly specify the scope of the service.
HCP Qualification & Onboarding
All healthcare professionals (HCPs) providing services through the Abi Proapp platform are required to undergo a comprehensive, multi-step onboarding and credentialing process, designed to uphold clinical integrity, user safety, and regulatory compliance. This process includes the following core components:
Document Collection and Primary Source Verification
As part of our credentialing protocol, each HCP must submit the following required documentation, which is meticulously reviewed and validated:
- Medical License Verification: Every license is verified directly with the relevant national or regional medical regulatory authority, ensuring it is active, valid, and unrestricted.
- Government-Issued Identification: A valid government-issued ID is collected to confirm identity and legitimacy.
- Curriculum Vitae (CV) or Resume: A full professional, updated CV is required.
Country-Specific Documentation:
Depending on the country of practice, additional documents may be collected to strengthen verification and demonstrate professional compliance. These may include:
- Criminal Record Checks: To confirm a clean professional and legal background.
- Proof of Malpractice Insurance / Professional Indemnity: Ensures coverage and accountability in clinical practice.
- Degree Certificates: Verification of medical degrees and qualifications.
- Specialization Certificates: Proof of specialty training and board certifications.
- Language Proficiency Certificates: Particularly relevant in multilingual countries, to ensure HCPs can communicate effectively with patients.
Other Regulatory or Compliance Documents: Depending on local requirements, such as continuing education certifications or professional affiliations.
By collecting both mandatory and optional documentation, our credentialing process provides a thorough and multi-layered verification, ensuring that only qualified and trustworthy HCPs are accepted onto our platform.
Structured Onboarding, Training, and Evaluation
After documentation validation, each HCP proceeds through a structured onboarding program aligned with Abi’s digital care delivery model:
- Signed Legal Agreement: All providers must execute our Terms & Conditions and the Data Protection and Privacy Policy and Notice, which include telemedicine-specific responsibilities, data privacy obligations, and service protocols. This legal agreement ensures HCPs understand their professional and regulatory responsibilities when providing care through our platform.
- Abi Global Clinical Guidelines and Country-Specific Operational and Clinical Guidelines: These provide the foundational medical framework for HCPs to answer a wide range of health-related questions from Abi customers and patients. They focus on clinical judgment, evidence-based responses, and professional conduct. Local guidelines detail procedures for starting, conducting, and ending consultations, as well as rules for issuing prescriptions, sick leave certificates, and referrals based on local regulations.
- Training: HCPs must complete mandatory training modules via a secure centralized clinical training platform, where their progress is verified through completion certificates. The Care Quality (CQ) team utilizes integrated tracking tools to maintain real-time visibility into overall completion percentages, individual module status, and specific areas requiring further attention. These modules cover the following essential topics:
- Abi Global Health Model & Scope: Comprehensive orientation on the company’s working model, international reach across various markets, and the organizational scope of digital health delivery.
- Abi ProApp Platform Orientation: Step-by-step guidance on navigating the platform, managing cases, and using core features.
- Text Consultation Protocols: How to respond to patient queries via text, including tone, documentation, and triage best practices.
- Video Consultation Training: Conducting secure and effective video consultations, including call setup, consultation flow, wait times and documentation.
- Prescription Management: How to add prescriptions in compliance with local regulations.
- Payment Process Overview: Understanding how payments are calculated, processed, and reflected in case histories.
- Professional Conduct & Documentation Best Practices: Guidance on maintaining confidentiality, professional behavior, accurate documentation, and following clinical protocols.
Clinical Simulation and Testing:
HCPs complete simulated medical cases in a controlled environment to assess:
- Clinical judgment and decision-making
- Communication and patient reassurance skills
- Adherence to triage and documentation protocols
Simulations use realistic scenarios based on actual user cases, selected by our clinical team. These exercises allow providers to demonstrate their readiness and apply clinical judgment and communication skills before interacting with real patients.
Live Evaluation via Video Consultation
As a final stage of onboarding, HCPs participate in a face-to-face video consultation with a trained evaluator. This session serves as a live training opportunity and an "in-person" meeting, allowing the HCP to:
- Platform Mastery: Explore the ProApp platform in detail and demonstrate technical fluency in a live environment.
- Direct Mentorship: Resolve any remaining doubts and receive immediate guidance from the clinical team.
Feedback and Eligibility Confirmation:
Following evaluations, HCPs receive personalized feedback from the CQ team, which includes MD staff and platform quality officers. Feedback highlights strengths, areas for improvement, and guidance on best practices. Only HCPs who meet Abi’s clinical, technical, and operational standards are approved to serve real users on the platform.
Continued Education
In the event of new information, HCPs are required to complete further online training courses through Abi’s training platform to ensure their knowledge and skills remain aligned with Abi’s clinical guidelines, evidence-based practices, and operational standards. Every time a new service is launched or an existing feature of the app is modified, HCPs are promptly notified and provided with updated training materials. These resources include guidance on new workflows, clinical protocols, and best practices to ensure seamless adoption and high-quality service delivery.
In addition to structured training, HCPs have continuous access to support for any questions or doubts they may have, via Abi’s medical team contact through email or following in-app case flagging. This ensures timely clarification, reinforces correct clinical practices, and supports the consistent application of standards across all consultations. HCPs are expected to demonstrate competency following training for every new service or feature before engaging further with users, ensuring they are fully prepared to deliver safe, effective, and high-quality care.
This approach to continued education combines proactive training, real-time support, and performance verification, enabling HCPs to stay up-to-date with evolving services and maintain clinical excellence across all platforms and regions.
Ongoing Clinical Performance Monitoring
Onboarding does not mark the end of evaluation. All active HCPs are subject to continuous quality assurance monitoring led by the Care Quality (CQ) team:
- Metrics Monitoring
We maintain a comprehensive and continuous metrics monitoring framework to ensure high clinical quality, operational efficiency, and a consistent user experience across all services and geographies. Metrics are reviewed routinely and systematically, with defined daily and bi-weekly review cycles, enabling both real-time operational oversight and longer-term trend analysis.
1. Core Quality and Performance Metrics
We routinely monitor high-level performance indicators, including but not limited to:
- User Feedback: Users provide ratings after each consultation to indicate how effectively HCPs address their concerns, helping us measure both clinical effectiveness and overall service quality. These ratings reflect the user’s perception of communication, helpfulness, and satisfaction. We enforce a strict minimum threshold of 4.7 stars (on average), and any average rating below this triggers immediate review and corrective action. Ratings capture the user’s subjective experience and trust, providing a direct measure of satisfaction. HCPs with lower ratings are automatically deprioritised by our AI triage system, ensuring that higher-rated HCPs are prioritised. This approach allows our medical team to promptly address concerns, provide timely feedback, and maintain a consistent, high-quality service for all users.
- AI-Generated Ratings: Independently, our AI evaluates each HCP consultation across multiple objective and subjective criteria, including spelling and grammar, opening and closing (greetings and well-wishes), empathy, reassurance, clarity, friendliness, handling of symptoms, relevance, efficiency, urgency, and visit justification. These ratings provide a standardized and consistent measure of HCP performance, helping to identify quality issues, inform training, and optimize consultations across partners, countries, and service types.
- The Abi Medical Team conducts audits on 100% of AI-tagged cases and low-rated cases, ensuring adherence to evidence-based medicine and clinical guidelines.
- AI Support: Abi’s AI system scans 100% of cases for emergency situations, suicidal ideation, and other critical concerns. HCPs can flag cases for additional support, ensuring that any urgent situations are handled promptly.
- Clinical accuracy, ensuring that consultations and clinical decisions align with accepted medical standards and evidence-based practices.
- Adherence to clinical and operational protocols including prescribing guidelines, and escalation procedures, for example.
- User communication quality, assessing clarity, tone, empathy, professionalism, and completeness of interactions between healthcare professionals and users.
- Service consistency, ensuring a uniform level of service quality across partners, countries, and consultation modalities.
2. Daily Operational Metrics Review
The following metrics are reviewed on a daily basis by the Care Quality team to enable rapid identification of issues and timely corrective action:
2.1 Consultation Volumes
- Total case numbers, broken down:
- By partner
- By country
- By case type, including:
- Text consultations
- Video consultations
- Prescription-only consultations
This analysis is conducted across all regions and markets where we operate, enabling visibility into demand patterns and partner-specific performance.
2.2 Consultation Match Times
- Consultation match time: the time elapsed between a user requesting a consultation and an HCP successfully connecting with the user. These metrics are monitored to ensure timely access to care and to identify capacity constraints or regional imbalances.
2.3 HCP Response Times
- Response time: the time it takes for the HCP to respond to the user after the initial connection has been established.
- This metric supports monitoring of engagement quality, responsiveness, and adherence to service-level expectations.
2.4 Consultation Resolution Rates
Percentage of consultations not resolved, including:
- Clinical reasons (e.g. need for in-person assessment, referral, or escalation)
- Technical issues
- User disengagement or abandonment
Root-cause analysis is conducted where non-resolution rates exceed expected thresholds, enabling targeted improvements.
2.5 HCP Participation and Capacity
Number of active HCPs participating on a weekly basis:
- By project
- By country
This metric supports workforce planning, capacity management, and partner performance evaluation.
3. AI-Driven Metrics Review
In addition to daily monitoring, our AI Lab produces a comprehensive, metrics overview covering all countries and service lines. This includes:
- Cross-country and cross-partner performance comparisons
- Trend and pattern analysis across all consultation types
- HCP participation trends and utilisation rates
- Overall user engagement metrics, including repeat usage and consultation completion trends
These AI-supported insights allow us to identify emerging risks, operational inefficiencies, and opportunities for optimisation at scale.
HCP Support and Performance Feedback
Regular performance reviews and constructive feedback are essential to help HCPs maintain clinical excellence and stay aligned with evolving standards. To provide continuous support, each HCP has a designated contact within our medical team at Abi, who serves as their reference for guidance and consultation.
HCPs can flag cases directly from the app whenever they encounter concerns regarding technical issues, inappropriate platform use by users, repeated prescription requests, or questions about handling a specific case. Each flagged case is monitored and reviewed by our medical team and care quality controllers, who assess the situation and take appropriate action, ensuring quality and safety are maintained.
In addition to in-app case flagging, HCPs can contact the medical team via email for guidance or queries. The team responds within 48 hours, depending on enquiry volume, providing timely, personalised support. This multi-channel approach ensures HCPs receive ongoing mentorship, rapid clarification, and structured feedback to maintain high-quality clinical standards while navigating complex or unusual cases.
Creation of a Public Professional Profile
Once onboarding is complete, a public-facing professional profile is created. This profile includes:
- Full name and professional headshot
- Country/location (if applicable)
- Verified medical license (where applicable)
- Medical specialties or areas of focus
- Languages spoken
- Educational background, including medical degree and specialty training institutions
These profiles are automatically created based on the information HCPs share with Abi, reviewed by the Care Quality team, and can be viewed by users once an HCP claims a case, letting them see who is attending to their medical concern.
Ongoing Biannual Quality Assurance Reviews
To ensure that all healthcare professionals providing telemedicine services through Abi consistently meet our quality, safety, and compliance standards, Abi conducts biannual Quality Assurance (QA) reviews for every active HCP.
These reviews are structured around three complementary audit pillars and are performed every six months per HCP, with tracking and documentation managed through internal systems. All audits are conducted in full compliance with applicable data protection and privacy regulations in each region (including GDPR and relevant local requirements).
1. Credentialing and Profile Review
This component ensures that each HCP remains appropriately licensed, documented, and accurately represented across all Abi systems.
Scope:
- Review of licenses, documentation, internal records, public profiles, and country-specific requirements
- Applies to all HCPs, including those licensed in multiple countries
- The review frequency is every 6 months per HCP
Review Workflow:
- Verify medical license validity (must be active and not expiring within the next 6 months)
- Audit the HCP’s document folder (containing CV, Official ID and additional qualifications or licenses depending on the country’s regulatory processes)
- Update internal Admin records to reflect activity status
- Update Abi's CRM system contact information and add review notes to keep track of individual Professional profile changes
- Verify Professional profile accessible to users (photo, bio, specialties, credentials, live link accuracy)
- Re-set the next Abi's CRM system calendar alert to be automatically informed of when the next audit for that particular HCP is due
- Complete and save the QA checklist (PDF) to the HCP folder
Mandatory Document Folder Contents:
- Valid medical license
- Valid government-issued ID
- CV / resume
- Country-specific checks (e.g., DBS for the UK, Garda Vetting for Ireland)
- Most recent QA checklist
This process ensures ongoing regulatory compliance and alignment across all internal and public-facing systems.
2. Performance Monitoring & KPIs
Performance monitoring is a core subsection of the QA review, using quantitative and qualitative indicators to assess the quality, consistency, and safety of each HCP’s activity. Performance KPIs Reviewed Include:
Clinical & Quality Metrics
- Evidence-based clinical responses
- Adherence to clinical guidelines, professional and operational standards
- AI-based evaluation scores (grammar, clarity, completeness, empathy, tone, rating)
- User satisfaction ratings
Case Handling & Engagement Metrics
- Total number of cases handled
- Average daily cases since onboarding
- Breakdown by service type (text, video, voice, form-based assessments, B2B vs D2C)
- Response rate (answered cases / total notifications)
- Skip ratio, expired ratio, cancelled ratio
- Percentage of unresolved cases
- Percentage of unsuccessful video consultations (e.g., technical issues)
- Time spent per case, split by case type
Clinical Output Metrics
- Number of prescriptions issued (average per case)
Percentage of declined prescriptions (Form RX)
Referrals and sick notes issued
Operational Alerts & Controls
- Monitoring of case concentration per country (e.g., % of total country cases handled by the HCP)
Adjustment of notifications when case distribution thresholds are exceeded
Identification of inactive or underutilized HCPs (with follow-up via Admin and Abi's CRM system updates)
Performance audits may also be conducted ad hoc, upon request, for specific HCPs or in response to identified risks or anomalies.
3. Case Audits (Text, Video Consultations, Form-based Assessments)
Case audits involve qualitative review of real consultations to ensure high standards of communication, clinical appropriateness, and professional conduct.
Text Consultations – Audit Criteria
Communication & Tone:
- Grammar, spelling, and clarity
- Appropriate opening and closing
- Empathy and reassurance
- Friendly and professional tone
Clinical Content:
- Relevance and medical accuracy
- Efficiency in questioning (avoiding unnecessary follow-ups)
Appropriate urgency handling
Clear justification for in-person referrals - Guidance for symptom management when referral is advised
Video Consultations – Audit Criteria: All text consultation criteria apply, plus:
Consultation Conduct & Environment:
- Privacy and confidentiality
- Professional background, attire, and posture
- Lighting, camera placement, and eye contact
- Minimal background noise and distractions
Focus and engagement throughout the consultation
- Duration within recommended ranges
- Handling of technical issues
Clinical Completeness:
- Quality and usefulness of consultation summaries
- Appropriate use of AI notes
- Correct issuance of prescriptions, sick notes, or referrals
Prescriptions in Video Consultations
- Medical appropriateness
Clear dosage, frequency, and duration instructions
Aggregated Audit Outcomes
Across audits, Abi tracks aggregated metrics such as:
- Average consultation duration (by modality)
- Total doctor time per case
- Proportion of consultations with communication, privacy, or clinical issues
Frequency and type of technical issues - Overall clinical output trends
These aggregated insights inform platform improvements, training updates, and risk mitigation strategies.
Data Protection & Confidentiality
All QA reviews and audits are conducted in strict accordance with regional data protection regulations, ensuring that patient data, HCP data, and audit materials are accessed, stored, and processed securely and lawfully.
Performance Feedback & Risk Management Strategy
Abi Global Health employs a comprehensive risk management framework to ensure the safety, quality, and reliability of its services. This framework includes the systematic identification, assessment, and mitigation of risks related to clinical and operational processes:
- Immediate Audit of Clinical Cases
Cases flagged for emergencies or other critical situations are audited immediately. As mentioned above, our HCPs can flag cases directly from the app whenever they identify concerns, including technical issues, inappropriate platform use by users, repeated prescription requests, or uncertainties about handling a specific case. Each flagged case is promptly reviewed by our medical team and care quality controllers, who take appropriate actions based on the nature and severity of the issue. Actions may include:
- Reaching out to warn or deactivate users if their behavior poses a risk.
- Verifying and correcting clinical advice to ensure it is sound and aligned with the emergency situation.
- Contacting country-specific authorities if the case poses a potential risk of harm to the user or others.
This process ensures that urgent or high-risk cases receive immediate attention, that clinical standards are strictly maintained, and that any necessary interventions are implemented swiftly to protect patient safety and public health.
- Daily Audit of Performance Issues
Daily audits are conducted on cases flagged for suboptimal performance to ensure timely intervention and corrective action. HCPs can flag cases directly from the app when they encounter issues such as technical problems, repeated prescription requests, inappropriate platform use by users, or uncertainties regarding case handling. Each flagged case is reviewed by our medical team and care quality controllers to:
- Verify that the clinical advice provided was accurate and aligned with best practices.
- Provide targeted feedback or guidance to HCPs where performance gaps are identified.
- Escalate systemic or recurring issues to the relevant teams for process improvement or training.
- Take action to protect users or public safety if flagged cases reveal behavior that could cause harm, including warning or deactivating users and contacting country-specific authorities if needed.
This daily audit process ensures that performance issues are addressed promptly, supporting continuous quality improvement, HCP development, and safe, reliable service delivery across all consultation types and regions.
- Routine Evaluation of Healthcare Provider Performance
HCP performance is regularly evaluated to ensure adherence to Abi’s clinical guidelines and evidence-based practices. Evaluations draw on user ratings, AI-generated assessments, and flagged case reviews, with daily and immediate audits addressing any performance or safety concerns. HCPs receive personalised guidance from their dedicated medical team contact, ensuring timely feedback, corrective action, and continuous support to maintain clinical excellence and high-quality care across all services and regions. - Automated Identification of Irregularities
Our system continuously monitors HCP consultations to automatically detect potential irregularities that could affect clinical quality, compliance, or user safety. Examples of detected irregularities include:
- Deviation from clinical guidelines or evidence-based practices.
- Sharing of personal or sensitive user data inappropriately.
- Incomplete or unclear documentation of symptoms, advice, or visit justification.
- Unusual patterns in prescribing or consultation behavior, such as repeated prescription requests or unusually rapid/frequent case closures.
When an irregularity is identified, we can further explore the reasons and trends via AI summary reviews or by revising the consultation recordings. Corrective actions may include:
- Direct feedback or guidance to the HCP.
- Case follow-up to ensure clinical advice was accurate and safe.
- Escalation for potential risk to users, including deactivation or warnings where necessary.
By automating the identification of irregularities, Abi ensures rapid detection and resolution of issues, protecting patient safety, maintaining adherence to clinical standards, and supporting continuous quality improvement across all consultations and regions.
- Data Protection & GDPR Compliance
All HCP data is stored securely, in compliance with GDPR and other relevant data protection regulations, ensuring patient privacy is upheld at all times.
Intervention Strategy
In the event of identified risks, immediate corrective actions, such as additional training or performance reviews, are implemented. In extreme cases, removal from the service may be considered after a thorough assessment by the Chief Medical Director.
To maintain clinical excellence, Abi utilizes a tiered intervention strategy to address non-compliance and performance gaps identified during monitoring, where the level of contact and corrective action depend on the clinical or operational impact of the issue:
- Low-Level Issues: Feedback is provided via email notification, serving as a formal notice to the HCP to correct minor deviations in tone, documentation, or response times.
- Mid-Level Issues: These require mandatory retraining; depending on the nature of the issue, this involves completing online modules via Abi’s training platform or participating in a live session with an Abi staff member to demonstrate competency.
- High-Level Escalation: Reserved for significant or recurring non-compliance, this stage includes:
- Temporary Service Pause: An immediate suspension of the HCP's ability to claim cases while the issue is reviewed by senior management.
- First Formal Warning: A formal ultimatum requiring a commitment to re-comply with all guidelines and complete intensive retraining.
- Second Formal Warning & Termination: A final warning that results in permanent removal from the platform after a thorough assessment by the Chief Medical Director.
- Acknowledgement Requirement: For all levels of intervention, the HCP must provide a written reply of acknowledgement that explicitly confirms their understanding of the feedback and a formal commitment to adhere to Abi’s clinical and operational guidelines moving forward.
Why This Matters to You
By partnering with Abi, you gain access to a rigorously credentialed and continuously monitored network of healthcare professionals you can trust to deliver safe, high-quality care. Our structured processes—spanning verification, training, ongoing audits, and risk management—directly protect your brand’s reputation while ensuring that every user interaction meets regulatory, ethical, and clinical standards.
This means fewer compliance risks, greater confidence in service delivery, and the assurance that your users are receiving care from fully licensed, well-vetted professionals. Our transparent, auditable approach allows you to demonstrate due diligence and maintain trust with your stakeholders, so you can focus on scaling your business while we safeguard quality and clinical excellence on your behalf.
Any Questions?
For audit requests, compliance reports, or further assurance documentation, contact: medical@abi.ai

